Table of Contents
Introduction
Obinutuzumab, marketed as Gazyva in the United States and Gazyvaro in Europe, represents a major advancement in targeted cancer therapy. It’s a humanized monoclonal antibody designed to recognize and attack the CD20 antigen present on B lymphocytes. This mechanism makes it highly effective in treating Chronic Lymphocytic Leukemia (CLL) and Follicular Lymphoma (FL)—two common types of B-cell malignancies.
However, like most monoclonal antibody therapies, obinutuzumab is not free from side effects. Understanding these side effects—both common and serious—helps clinicians manage them better and empowers patients to stay informed and safe during treatment.
This article provides a comprehensive, updated, and patient-friendly overview of obinutuzumab side effects, backed by the latest clinical evidence and expert guidelines as of 2025.
What Is Obinutuzumab and How Does It Work?
Obinutuzumab belongs to the anti-CD20 antibody class, similar to rituximab but engineered for enhanced efficacy. It binds to the CD20 antigen found on the surface of B-cells and induces their destruction through mechanisms such as:
- Antibody-dependent cellular cytotoxicity (ADCC)
- Complement-dependent cytotoxicity (CDC)
- Direct induction of apoptosis (programmed cell death)
By eliminating malignant and normal B-cells, obinutuzumab helps control cancer cell proliferation. However, this immune-mediated depletion of B-cells also contributes to many of its side effects, particularly those involving immune suppression and infection risk.
Overview of Obinutuzumab Side Effects
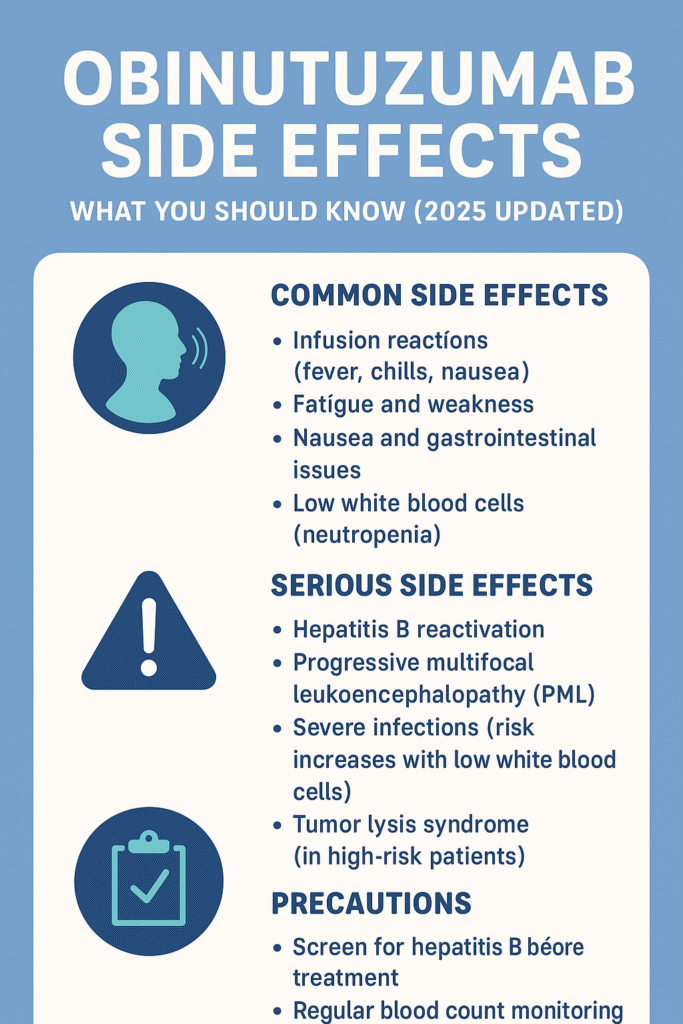
Like other anti-CD20 monoclonal antibodies, obinutuzumab side effects can range from mild infusion-related reactions to potentially life-threatening complications such as hepatitis B reactivation and progressive multifocal leukoencephalopathy (PML).
Broadly, these side effects can be categorized as:
- Common and manageable side effects
- Serious and life-threatening adverse reactions
- Delayed or long-term immune effects
Understanding each category helps healthcare providers anticipate and mitigate risk during therapy.
1. Common Obinutuzumab Side Effects
Most patients undergoing treatment with obinutuzumab experience mild to moderate side effects that can be managed with supportive care or dose adjustments. These usually occur during or shortly after infusion.
a. Infusion-Related Reactions (IRRs)
These are the most common obinutuzumab side effects , particularly during the first infusion.
Symptoms may include:
- Fever or chills
- Fatigue
- Nausea
- Hypotension (low blood pressure)
- Difficulty breathing or chest tightness
- Rash, hives, or itching
Frequency: Clinical trials report IRRs in up to 65% of patients during the first infusion, with a notable decline in later cycles.
Management:
Premedication with corticosteroids, acetaminophen, and antihistamines, along with slow infusion rates, significantly reduces IRR severity. If a reaction occurs, the infusion can be paused and restarted at a slower rate once symptoms resolve.
b. Fatigue and Weakness
Many patients report persistent tiredness or general weakness during treatment. This may be related to immune system activation, reduced red blood cell counts, or general stress from therapy.
Management Tips:
- Maintain adequate hydration and nutrition
- Incorporate light physical activity
- Monitor hemoglobin levels to rule out anemia
c. Nausea, Vomiting, and Gastrointestinal Disturbances
Digestive issues are common, including:
- Nausea or vomiting
- Diarrhea or constipation
- Mild abdominal pain
These symptoms are often temporary and can be managed with dietary adjustments or antiemetic medications. Staying hydrated and eating small, balanced meals can help.
d. Musculoskeletal Pain
Some patients experience joint pain, muscle aches, or back discomfort following infusions. These are typically mild but can affect quality of life.
Management: Over-the-counter pain relievers (e.g., acetaminophen) and warm compresses are usually sufficient.
e. Headache and Dizziness
These symptoms often occur transiently after infusion and are linked to immune or blood pressure fluctuations.
Tip: Report persistent headaches, especially if associated with vision changes or severe nausea, as these may indicate more serious neurological issues.
2. Hematologic Side Effects: Low Blood Cell Counts
Because obinutuzumab targets B-cells, it can also affect the bone marrow’s ability to produce blood cells.
a. Neutropenia (Low White Blood Cell Count)
Neutropenia is among the most significant hematologic side effects.
It can occur early or late during therapy, predisposing patients to serious infections.
Clinical data:
- Up to 40% of patients develop some degree of neutropenia.
- Severe (Grade 3–4) neutropenia occurs in 10–20% of cases.
Management:
- Regular complete blood count (CBC) monitoring
- Administration of granulocyte-colony stimulating factors (G-CSF) if needed
- Preventive antibiotics for high-risk cases
b. Thrombocytopenia (Low Platelet Count)
Acute or delayed thrombocytopenia can cause easy bruising or bleeding.
Symptoms to watch for:
- Nosebleeds
- Gum bleeding
- Blood in urine or stool
- Prolonged bleeding from cuts
Clinical note:
Severe thrombocytopenia can occur within 24 hours of the first infusion, though this is rare.
c. Anemia (Low Red Blood Cell Count)
Chronic anemia may develop over multiple cycles, leading to fatigue, pallor, and shortness of breath.
Management:
- Monitor hemoglobin levels
- Provide iron or erythropoietin therapy if indicated
3. Serious and Life-Threatening Side Effects
While most side effects are manageable, some rare but serious reactions require immediate medical attention.
a. Hepatitis B Virus (HBV) Reactivation
Because obinutuzumab suppresses B-cell immunity, it can reactivate latent hepatitis B infections, even in patients previously recovered from HBV.
Risk: Potentially fatal liver failure.
Prevention: All patients should undergo HBV screening before treatment. Antiviral prophylaxis (e.g., entecavir or tenofovir) is recommended for at-risk patients.
Monitoring: Continue liver function tests and viral load monitoring during and after therapy.
b. Progressive Multifocal Leukoencephalopathy (PML)
PML is a rare but potentially fatal brain infection caused by reactivation of the JC virus in immunocompromised patients.
Symptoms include:
- Vision problems
- Weakness on one side of the body
- Confusion or speech difficulties
If suspected, obinutuzumab should be discontinued immediately, and MRI and CSF analysis should be performed.
c. Severe Infections
Patients may experience bacterial, viral, or fungal infections, sometimes leading to sepsis. Common infections include:
- Pneumonia
- Bronchitis
- Urinary tract infections (UTIs)
Prevention:
- Maintain good hygiene and avoid crowded places
- Promptly report fever or sore throat
- Consider prophylactic antibiotics if neutropenia is prolonged
d. Tumor Lysis Syndrome (TLS)
TLS occurs when rapid tumor cell destruction releases intracellular contents into the bloodstream, leading to electrolyte imbalances and kidney dysfunction.
Symptoms:
- Nausea, vomiting
- Irregular heartbeat
- Muscle cramps
- Reduced urine output
Prevention:
- Adequate hydration
- Use of uric acid-lowering agents such as allopurinol or rasburicase
- Frequent lab monitoring during initial cycles
4. Long-Term and Delayed Side Effects
Long-term therapy with obinutuzumab can lead to prolonged immune suppression due to delayed B-cell recovery. This increases susceptibility to infections and reduces vaccine responses.
Key points:
- Avoid live vaccines during and up to 12 months after therapy.
- Some patients may experience hypogammaglobulinemia (low antibody levels), requiring IV immunoglobulin replacement.
- Regular follow-up with oncologists or immunologists is essential to track immune recovery.
5. Less Common obinutuzumab side effects
A few rare but noteworthy obinutuzumab side effects include:
- Allergic reactions: true anaphylaxis is rare but possible.
- Cardiac events: chest pain or arrhythmias during infusion in susceptible patients.
- Secondary malignancies: rare and causality uncertain, but continuous surveillance is prudent.
- Skin reactions: rash, itching, or localized redness, generally mild.
Monitoring and Managing Obinutuzumab Side Effects
Pre-Treatment Evaluation
Before starting obinutuzumab, healthcare providers should:
- Screen for hepatitis B (HBsAg and anti-HBc).
- Assess complete blood counts and organ function.
- Review current medications and comorbidities.
- Provide counseling about side effect recognition and management.
During Treatment
- Administer premedications (steroids, antihistamines, antipyretics).
- Start with a slow infusion rate, especially for the first dose.
- Monitor vital signs and symptoms throughout the infusion.
- Perform frequent blood tests to track hematologic toxicity.
Post-Treatment Care
After therapy completion:
- Continue monitoring for infections and delayed cytopenias for several months.
- Avoid live vaccines until B-cell recovery is confirmed.
- Encourage prompt medical consultation for any new neurological or hepatic symptoms.
Patient Education and Safety Tips
Educating patients plays a crucial role in improving outcomes. Here are practical tips:
✅ Report any fever, chills, or shortness of breath immediately.
✅ Stay hydrated and follow a balanced diet.
✅ Avoid contact with sick individuals during therapy.
✅ Maintain consistent follow-ups and lab appointments.
✅ Inform your healthcare provider before taking any new medications or vaccines.
Comparing Obinutuzumab with Rituximab
While both drugs target CD20, obinutuzumab differs structurally and functionally:
| Feature | Obinutuzumab (Gazyva) | Rituximab (Rituxan) |
| Type | Humanized monoclonal antibody | Chimeric monoclonal antibody |
| Mechanism | Type II CD20 binding — induces stronger direct apoptosis | Type I CD20 binding — relies more on CDC |
| Infusion Reactions | Slightly more frequent initially | Less intense but still common |
| Hematologic Toxicity | Higher risk of neutropenia/thrombocytopenia | Moderate |
| Efficacy (CLL/FL) | Superior progression-free survival in some studies | Standard reference |
While obinutuzumab may show enhanced anti-tumor activity, it can also cause more pronounced side effects, highlighting the need for careful monitoring.
Key Takeaways
- Obinutuzumab side effects range from common infusion reactions to rare, life-threatening complications.
- Monitoring and early intervention can prevent most severe events.
- Patients should maintain open communication with their healthcare team and report any unusual symptoms promptly.
- Long-term vigilance, especially for infection and liver function, is essential for safety.
Conclusion
Obinutuzumab continues to be a cornerstone therapy for CLL and FL, offering extended remission and survival benefits. Yet, the potential obinutuzumab side effects demand a balanced approach—vigilant monitoring, preventive strategies, and patient education.
With multidisciplinary care and informed patient participation, most side effects can be managed effectively, allowing individuals to receive the full therapeutic benefit while minimizing risks.