Table of Contents
Introduction
When managing hereditary tyrosinemia type 1 (HT-1), a rare but serious metabolic disorder, Nitisinone has emerged as a life-saving therapy. This medication, developed in the 1990s, revolutionized treatment by preventing the buildup of toxic byproducts in the liver and kidneys. However, like every powerful drug, patients and caregivers must understand the Nitisinone side effects that can occur during therapy.
This comprehensive guide explores:
- How Nitisinone works in the body
- Common and rare side effects
- Long-term safety concerns
- Tips for managing adverse reactions
- Frequently asked questions for patients and healthcare providers
By the end of this article, you will have an in-depth understanding of Nitisinone side effects, ensuring informed decisions and better health outcomes.
What is Nitisinone?
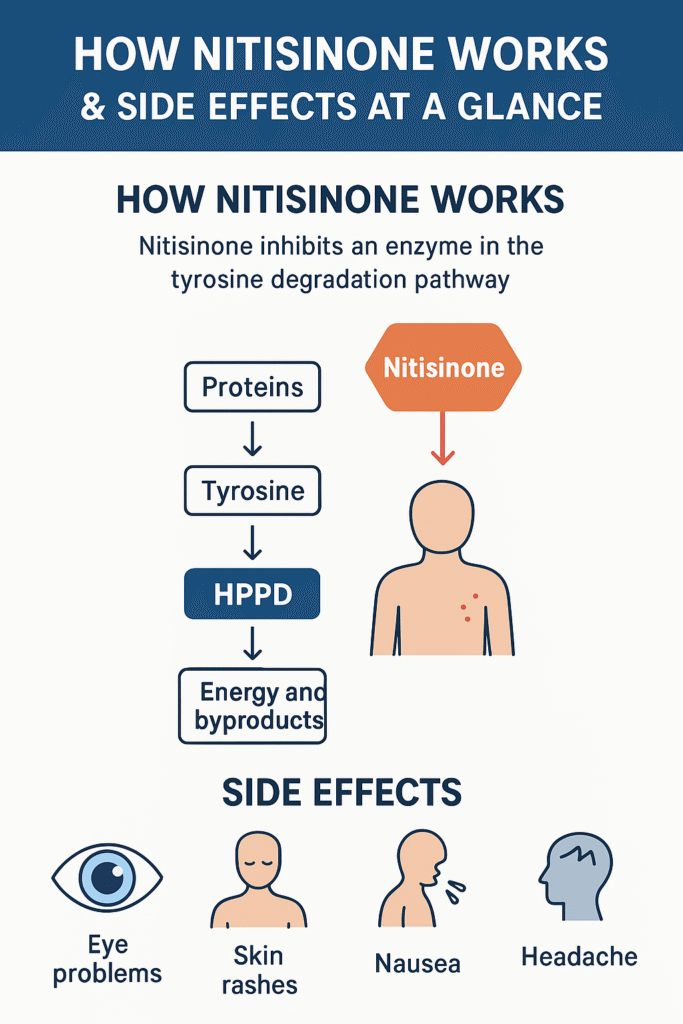
Nitisinone is a medication that works by inhibiting an enzyme called 4-hydroxyphenylpyruvate dioxygenase (HPPD), which plays a role in the tyrosine degradation pathway. In hereditary tyrosinemia type 1, a genetic deficiency in the enzyme fumarylacetoacetate hydrolase leads to the accumulation of toxic metabolites that damage the liver, kidneys, and sometimes the nervous system.
By blocking HPPD, Nitisinone prevents these harmful substances from forming, dramatically improving survival rates and reducing the need for liver transplantation.
Approved Uses of Nitisinone
- Hereditary Tyrosinemia Type 1 (HT-1): The main approved indication.
- Oculocutaneous Albinism Type 1B (OCA1B): Being studied as an investigational use.
- Other Research Areas: Alkaptonuria, tyrosinemia type II, and certain metabolic disorders.
While its therapeutic benefits are undeniable, long-term use comes with possible side effects that patients need to monitor carefully.
How Nitisinone Works in the Body
To understand the side effects of Nitisinone, let’s first look at how it interacts with the tyrosine metabolism pathway.
- Normally, dietary proteins are broken down into amino acids, including tyrosine.
- Tyrosine is further degraded into energy and metabolic byproducts.
- In patients with HT-1, toxic substances like fumarylacetoacetate and succinylacetone accumulate, damaging organs.
- Nitisinone blocks HPPD, stopping this breakdown early and preventing the toxic compounds from forming.
However, because this block also causes elevated blood tyrosine levels, one of the major concerns with Nitisinone is tyrosinemia-induced complications — including eye, skin, and neurological problems.
Common Nitisinone Side Effects
Patients on Nitisinone often experience mild to moderate side effects, particularly related to increased tyrosine levels in the blood.
1. Eye Problems (Ocular Effects)
- Eye discomfort or pain
- Photophobia (sensitivity to light)
- Keratitis (inflammation of the cornea)
- Conjunctivitis (red, irritated eyes)
- Dryness or excessive tearing
2. Skin-Related Side Effects
- Skin rashes
- Itching (pruritus)
- Thickening of the skin on the palms and soles (keratoderma in rare cases)
3. Digestive System Complaints
- Nausea and vomiting
- Abdominal discomfort
- Loss of appetite
4. General Symptoms
- Fatigue
- Headache
- Dizziness
- Joint pain (arthralgia)
These side effects often result from high blood tyrosine levels. A special low-tyrosine, low-phenylalanine diet is usually recommended alongside Nitisinone to reduce these complications.
Rare but Serious Nitisinone Side Effects
Though less common, certain serious side effects can occur with long-term Nitisinone use.
1. Corneal Crystals
Some patients develop crystalline deposits in the cornea due to high tyrosine levels. This may cause blurred vision, eye irritation, or light sensitivity.
2. Developmental Delays in Children
Since the drug alters amino acid metabolism, some pediatric patients may experience delayed growth or neurological symptoms if blood tyrosine is not well controlled.
3. Neurological Complications
- Tingling or numbness
- Impaired reflexes
- Seizures (rare but reported in poorly controlled cases)
4. Liver and Kidney Concerns
Although Nitisinone protects against toxic damage, improper monitoring may still result in abnormal liver function tests or renal complications.
Long-Term Safety of Nitisinone
Nitisinone has been in use for more than two decades, and studies confirm its long-term survival benefits for patients with HT-1. However, prolonged use requires careful monitoring:
- Blood tyrosine levels should be checked regularly.
- Liver and kidney function tests are mandatory.
- Ophthalmic examinations are essential to detect early corneal changes.
Most side effects can be controlled with dietary adjustments and dose modifications, making Nitisinone relatively safe under medical supervision.
Managing Nitisinone Side Effects
Patients and caregivers should follow a structured plan to reduce the risks:
- Follow a Strict Diet
- Low-tyrosine, low-phenylalanine diet
- Avoid high-protein foods (meat, cheese, fish, eggs) without medical advice
- Use special medical formula for children
- Regular Medical Monitoring
- Frequent blood tests (tyrosine, phenylalanine, succinylacetone)
- Liver and kidney monitoring
- Eye checkups
- Report Symptoms Early
- Eye pain, blurred vision, or light sensitivity must be reported immediately
- Persistent nausea, fatigue, or skin changes should be monitored
- Caregiver Education
- Parents of children on Nitisinone should receive dietary training
- Schools should be informed of special dietary needs
Nitisinone Drug Interactions
While generally safe, Nitisinone may interact with other medications. Some potential interactions include:
- Vitamin C (ascorbic acid): May reduce blood tyrosine levels, requiring monitoring.
- Other amino acid supplements: Can worsen side effects.
- Drugs affecting liver enzymes: Require close observation.
Nitisinone and Pregnancy
There is limited research on the safety of Nitisinone during pregnancy. Doctors usually recommend:
- Avoiding Nitisinone unless benefits outweigh risks.
- Close monitoring if treatment is essential.
- A safe, low-tyrosine diet for expectant mothers.
Conclusion
Nitisinone has changed the lives of patients with hereditary tyrosinemia type 1, offering hope where liver failure was once inevitable. While its benefits are remarkable, awareness of Nitisinone side effects is essential for safe treatment.
By following a specialized diet, undergoing regular checkups, and reporting unusual symptoms promptly, patients can enjoy the full benefits of this groundbreaking therapy while minimizing adverse effects.
If you or a loved one is starting Nitisinone, always consult your healthcare team for personalized advice. Knowledge, monitoring, and proactive care are the keys to safe and effective treatment.