Table of Contents
Introduction: Breathing New Life into Pulmonary Fibrosis Treatment
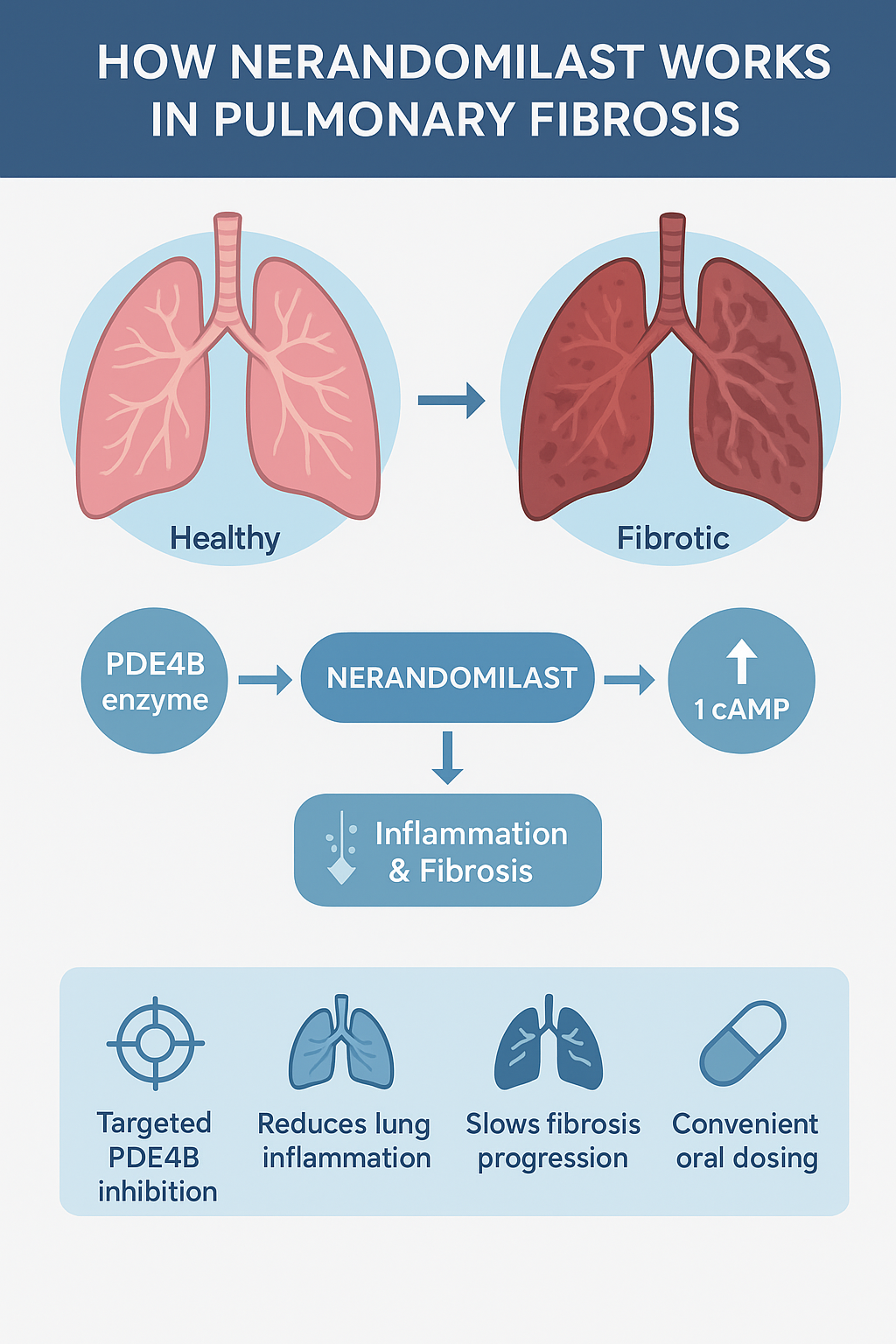
Progressive pulmonary fibrosis (PPF) and idiopathic pulmonary fibrosis (IPF) are chronic, life-limiting lung diseases that make it increasingly difficult to breathe. For decades, patients had limited treatment options, primarily pirfenidone and nintedanib, both of which slow – but do not stop – the progression of the disease.
Enter nerandomilast (BI 1015550) – a novel, oral phosphodiesterase 4B (PDE4B) inhibitor being developed as a potential game-changer in fibrosis management. With its targeted mechanism of action and encouraging clinical data, this investigational therapy is shaping up to be one of the most exciting developments in respiratory medicine in recent years.
What is Nerandomilast?
Nerandomilast is an investigational small-molecule drug designed to selectively inhibit phosphodiesterase 4B (PDE4B) – an enzyme involved in regulating inflammation and immune responses in lung tissue. Unlike traditional PDE4 inhibitors that affect multiple enzyme subtypes (often causing side effects such as nausea or vomiting), nerandomilast preferentially inhibits PDE4B, thereby maintaining a good balance of efficacy and tolerability.
Key Highlights:
- Generic name: Nerandomilast
- Development code: BI 1015550
- Drug class: Phosphodiesterase 4B (PDE4B) inhibitor
- Formulation: Oral tablet
- Indication under study: Progressive Pulmonary Fibrosis (PPF) and Idiopathic Pulmonary Fibrosis (IPF)
Understanding Pulmonary Fibrosis
Pulmonary fibrosis is a lung disorder characterized by progressive scarring (fibrosis) of lung tissue. Over time, the thickened and hardened lung tissue makes it increasingly difficult for oxygen to pass into the bloodstream, leading to symptoms such as:
• Difficulty breathing
• Persistent dry cough
• Fatigue
• Chest discomfort
In idiopathic pulmonary fibrosis (IPF), the cause remains unknown. However, chronic inflammation, abnormal wound healing, and immune dysregulation play a major role in the progression of fibrosis.
Currently available antifibrotic treatments help slow the decline in lung function, but there is an urgent need for treatments that halt or reverse the progression of the disease – a role that nerandomilast seeks to fill.
Mechanism of Action:
Step-by-Step Overview:
- PDE4B Enzyme Role:
The PDE4B enzyme breaks down cyclic AMP (cAMP), a messenger molecule that helps regulate inflammatory responses in lung tissue. - Inhibition by Nerandomilast:
Nerandomilast selectively inhibits PDE4B, leading to increased levels of cAMP within immune and structural lung cells. - Anti-Inflammatory Effect:
Higher cAMP levels suppress the release of inflammatory mediators like TNF-α and IL-1β, helping to reduce chronic inflammation in lung tissue. - Antifibrotic Effect:
Nerandomilast modulates fibroblast activity, potentially reducing excessive collagen deposition and slowing fibrosis progression. - Improved Lung Function:
By decreasing inflammation and scarring, it helps maintain or improve forced vital capacity (FVC) — a key marker of lung health.
Clinical Development
Phase 2 Clinical Findings
Early clinical studies of nerandomilast in patients with idiopathic pulmonary fibrosis (IPF) and other progressive fibrotic lung diseases have shown encouraging safety and efficacy. Participants taking nerandomilast showed stabilization or gradual decline in lung function (as measured by FVC) compared with placebo, suggesting its potential as monotherapy and combination therapy with standard antifibrotic drugs.
Key Observations:
- Improved Lung Function: Slower rate of FVC decline.
- Good Tolerability: Lower risk of gastrointestinal side effects compared to non-selective PDE4 inhibitors.
- Potential Synergy: May be safely combined with existing IPF therapies.
Benefits in Pulmonary Fibrosis
| Parameter | Potential Benefit |
| Inflammation control | Reduces chronic inflammation in the lungs |
| Fibrosis reduction | Slows scarring and stiffening of lung tissue |
| Lung function | Helps maintain FVC and oxygen exchange |
| Safety profile | Better tolerability than earlier PDE4 inhibitors |
| Administration | Easy once or twice daily oral dosing |
These combined effects make Nerandomilast a promising candidate in managing fibrotic lung diseases that currently have limited options.
Comparison with Existing Therapies
| Feature | Pirfenidone | Nintedanib | Nerandomilast |
| Mechanism | Antifibrotic, anti-inflammatory | Tyrosine kinase inhibitor | PDE4B inhibitor |
| Route | Oral | Oral | Oral |
| Primary Action | Slows fibrosis | Slows fibrosis | Targets inflammation + fibrosis |
| GI Side Effects | Moderate | Common | Mild (due to PDE4B selectivity) |
| Combination Use | Limited | Limited | Promising potential |
Nerandomilast’s unique mechanism and selective inhibition make it a potential next-generation therapy that complements, rather than replaces, existing antifibrotic drugs.
Nerandomilast’s Role in the Future of PPF and IPF Treatment
If clinical results continue to confirm its benefits, Nerandomilast could become:
- A first-line oral therapy for early-stage pulmonary fibrosis.
- A combination option for patients unresponsive to current antifibrotics.
- A preventive therapy for at-risk populations with early lung scarring patterns.
Beyond IPF, researchers are exploring Nerandomilast for other fibrotic lung diseases and chronic inflammatory respiratory disorders — potentially expanding its therapeutic footprint.
Safety and Side Effects
While safety data is still being evaluated, early findings suggest a favorable side-effect profile compared to broader PDE4 inhibitors like roflumilast.
Common Mild Side Effects Reported:
- Headache
- Nausea (less frequent than earlier PDE4 inhibitors)
- Mild diarrhea or fatigue
Rare or Serious Side Effects:
- Transient liver enzyme elevations
- Occasional dizziness
Most side effects have been dose-dependent and reversible, making Nerandomilast a well-tolerated option under investigation.
Ongoing Research and Future Outlook
The continued global research on Nerandomilast highlights its long-term potential to improve lung function, reduce hospitalizations, and enhance quality of life for patients with fibrotic lung diseases.
Future directions include:
- Phase 3 trials to confirm clinical benefits and safety.
- Combination studies with antifibrotic agents.
- Exploration of its effects in systemic sclerosis-associated interstitial lung disease (SSc-ILD) and other fibrotic conditions.
If results remain positive, regulatory submission and approval may be pursued in the near future, offering a much-needed therapeutic breakthrough.
Patient Perspective: A Ray of Hope
For individuals battling progressive pulmonary fibrosis, each breath is a challenge. New therapeutic candidates like Nerandomilast represent more than just scientific advancement — they symbolize hope for extended life, improved comfort, and renewed optimism.
Early reports of stable lung function and better symptom control provide patients and caregivers with tangible hope that the future of pulmonary care is changing for the better.
The Broader Impact
Pulmonary fibrosis doesn’t only affect the lungs; it impacts emotional well-being, physical endurance, and daily quality of life. With Nerandomilast, the global medical community moves one step closer toward transformative care that addresses both the physiological and emotional burdens of chronic lung diseases.
By focusing on targeted enzyme inhibition and balancing safety with efficacy, this innovative oral therapy may soon help patients breathe easier and live longer.
Conclusion
Nerandomilast is at the forefront of innovation in respiratory medicine. As a selective PDE4B inhibitor, it bridges the gap between inflammation control and antifibrotic therapy. With promising early data, improved tolerability, and convenient oral administration, it could redefine how physicians approach the management of progressive pulmonary fibrosis and idiopathic pulmonary fibrosis.
The journey from investigational candidate to approved therapy is ongoing – but one thing is certain: Nerandomilast offers a new breath of hope for patients with fibrotic lung disease.

2 thoughts on “Nerandomilast – A Breakthrough Hope for Progressive Pulmonary Fibrosis (2025)”